BIO’s Paris delegation strengthens Franco-American biotech ties
France’s government is putting €54 billion toward the growth of priority industries, including ...
Read More Dispatches from the BIO Agriculture & Environment Summit: the market outlook, plant biostimulants, animal vaccines, and more
The inaugural Biotechnology Innovation Organization (BIO) Agriculture & Environment Summit, April 17-18, 2024, ...
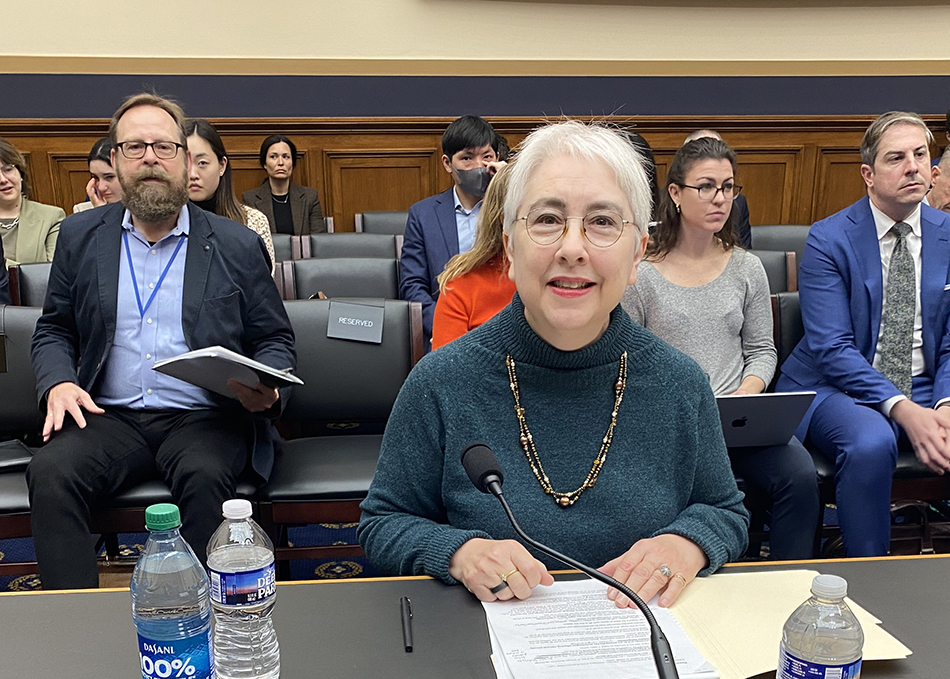
Read More Sanders launches politically motivated investigation into revolutionary, cost-effective diabetes and obesity medicines
Sen. Bernie Sanders (I-Vt.), Chair of the Senate Health, Education, Labor, and Pensions ...
Read More Limb Loss and Limb Difference Awareness Month: Amputee Coalition highlights advocacy wins, importance of community
During April’s Limb Loss and Limb Difference Awareness Month, the Amputee Coalition celebrates ...
Read More BIO members fly in, Member of Congress flies out
In April, the Biotechnology Innovation Organization (BIO) held its biggest “fly-in” since the ...
Read More U.S. biotech leadership is rooted in strong IP protection
For evidence of the link between biotech innovation and intellectual property protections, look ...
Read More EDITORS' CHOICE
Sanders launches politically motivated investigation into revolutionary, cost-effective diabetes and obesity medicines
Sen. Bernie Sanders (I-Vt.), Chair of the Senate Health, Education, Labor, and Pensions Committee, announced that he is launching an investigation into the pricing of ...
April 29, 2024
Read More LATEST NEWS
BIO Events
BIO’s Paris delegation strengthens Franco-American biotech ties
France’s government is putting €54 billion toward the growth of priority industries, including the biotech sector, learned a high-level delegation to Paris organized by the ...
April 30, 2024
Agriculture
Dispatches from the BIO Agriculture & Environment Summit: the market outlook, plant biostimulants, animal vaccines, and more
The inaugural Biotechnology Innovation Organization (BIO) Agriculture & Environment Summit, April 17-18, 2024, in Washington, D.C., brought together industry, regulators, and policymakers for a day ...
April 29, 2024
BIO's View
Sanders launches politically motivated investigation into revolutionary, cost-effective diabetes and obesity medicines
Sen. Bernie Sanders (I-Vt.), Chair of the Senate Health, Education, Labor, and Pensions Committee, announced that he is launching an investigation into the pricing of ...
April 29, 2024
Federal Policy
Limb Loss and Limb Difference Awareness Month: Amputee Coalition highlights advocacy wins, importance of community
During April’s Limb Loss and Limb Difference Awareness Month, the Amputee Coalition celebrates significant legislative victories, including new state laws enhancing prosthetic access. Since 1997, ...
April 29, 2024
BIO Events
BIO members fly in, Member of Congress flies out
In April, the Biotechnology Innovation Organization (BIO) held its biggest “fly-in” since the pandemic, while a Member of Congress “flew out” to visit a BIO ...
April 26, 2024
HEALTH
U.S. biotech leadership is rooted in strong IP protection
April 26, 2024
The next CRISPR frontier: delivery within the body
April 25, 2024
Company presentations at BIO 2024 inspire partnering
April 23, 2024
5 things to know for Primary Immunodeficiency Month
April 16, 2024
Biotech and One Health are key to controlling avian flu
April 15, 2024
Welcome, John F. Crowley!
Get to know John F. Crowley, the new President and CEO of the Biotechnology Innovation Organization (BIO), in our exclusive interview.
AGRICULTURE
U.S. biotech leadership is rooted in strong IP protection
April 26, 2024
Company presentations at BIO 2024 inspire partnering
April 23, 2024
John F. Crowley: ‘Biotechnology is another word for hope’
April 18, 2024
Biotech and One Health are key to controlling avian flu
April 15, 2024
Climate Change
Dispatches from the BIO Agriculture & Environment Summit: the market outlook, plant biostimulants, animal vaccines, and more
April 29, 2024
The inaugural Biotechnology Innovation Organization (BIO) Agriculture & Environment Summit, April 17-18, 2024, in Washington, D.C., brought together industry, regulators, ...
Read More Earth Day 2024 highlights need for plastic solutions
April 22, 2024
John F. Crowley: ‘Biotechnology is another word for hope’
April 18, 2024
Federal Policy
BIO members fly in, Member of Congress flies out
April 26, 2024
U.S. biotech leadership is rooted in strong IP protection
April 26, 2024
State Policy
Life Sciences PA recognizes John F. Crowley for biotech leadership
April 15, 2024
On April 10, Life Sciences PA awarded Biotechnology Innovation Organization (BIO) President & CEO John F. Crowley the Hubert J.P. ...
Read More Colorado PDAB could limit patient access to medicines
March 20, 2024
New Mexico legislature passes clean fuel standard
February 19, 2024
International
5 reasons for investor optimism at BIO-Europe Spring 2024
March 29, 2024
WTO Ministerial ends, no expansion of COVID IP waiver
March 4, 2024
Bio's View
BIO’s Paris delegation strengthens Franco-American biotech ties
April 30, 2024
France’s government is putting €54 billion toward the growth of priority industries, including the biotech sector, learned a high-level delegation ...
Read More Company presentations at BIO 2024 inspire partnering
April 23, 2024
John F. Crowley: ‘Biotechnology is another word for hope’
April 18, 2024